Total Knee Replacement Surgery
What is a Total Knee Replacement
A Total Knee Replacement also referred to as a Total Knee Arthroplasty is an operation to replace a knee joint that is affected by arthritis.
The procedure is a quality of life operation and is a highly successful operation.
Your new knee replacement can be expected to last for decades (90% are still functioning after 20 years).
Who are Candidates for Total Knee Replacement?
The procedure is usually recommended for older patients who suffer from pain and loss of function from arthritis or other knee degeneration and have failed to achieve satisfactory results from other conservative methods of therapy.
Each patient is assessed individually but Total Knee Replacement candidature is far greater than partial knee replacement and can include candidates who are:
- Suffering Pain, or
- Restricted Mobility that interferes with daily life
- Stiffness, Deformity or Swelling
These symptoms would usually have been present for many months or even years, often getting worse over time and are more common with older patients or severely arthritic patients
Benefits of Total Knee Replacement Surgery?
The decision to proceed with a Total Knee Replacement (TKR) is a cooperative one between you, your doctor, family and other medical professionals.
The benefits following surgery are the relief of symptoms of arthritis. These include
- Severe pain that limits your everyday activities including walking, shopping, visiting friends, getting in and out of a chair, gardening, etc.
- Pain waking you at night
- Deformity- either bowleg or knock knees
- Stiffness
Often TKR is a clear solution to help relieve symptoms and pain. Once the decision has been made to proceed with surgery, your doctor will explain the procedure and the risks (see below). A date for surgery is usually planned but can be deferred.
What is Total Knee Replacement?
Each knee is individual and knee replacements take this into account by having different sizes for your knee. If there is more than the usual amount of bone loss, sometimes extra pieces of metal or bone are added. Custom implants are occasionally required.
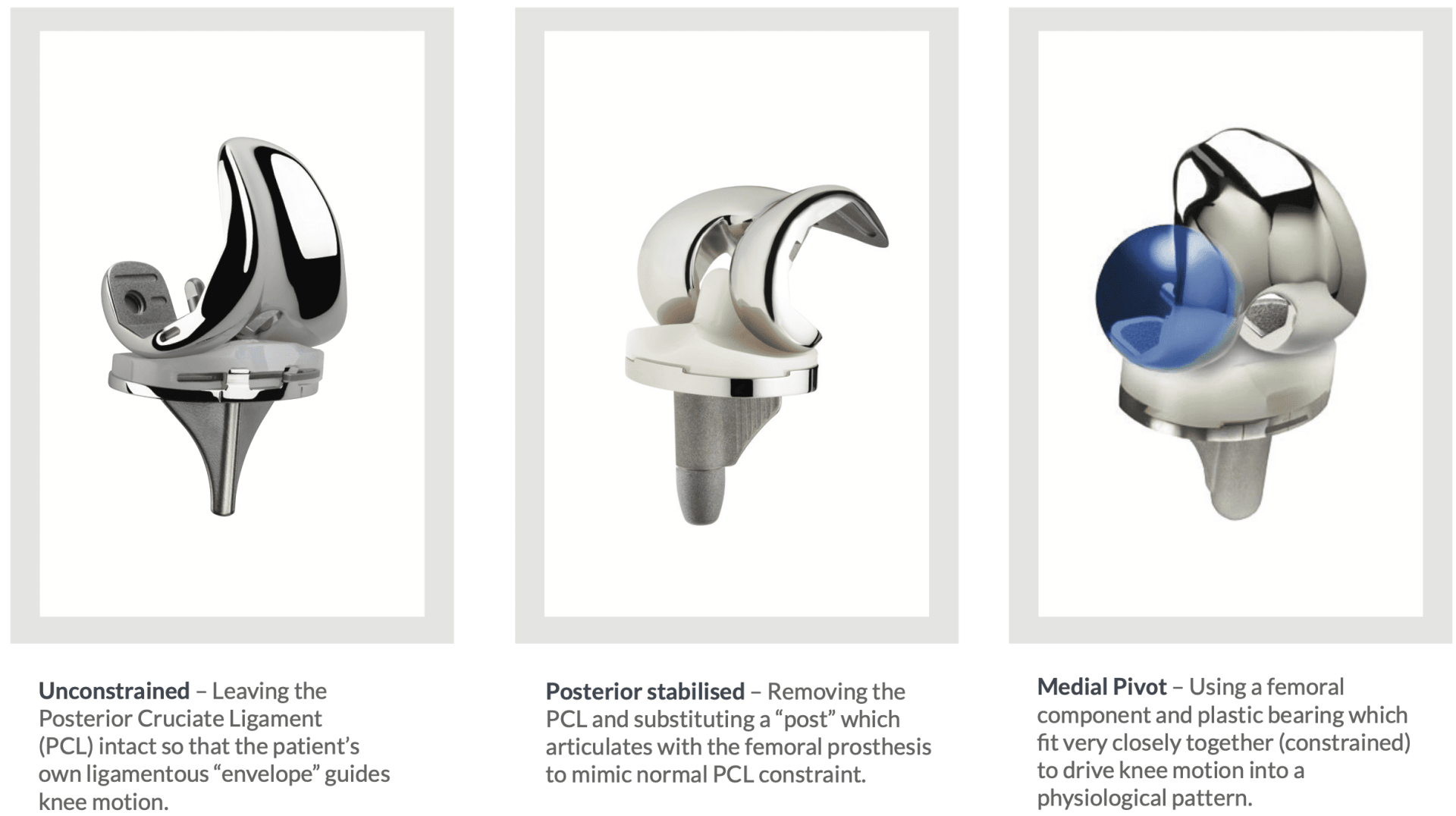
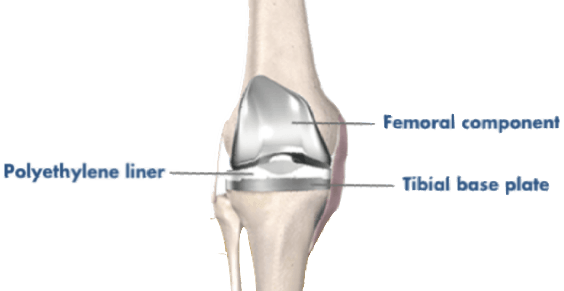
Total Knee Replacement surgery involves resurfacing the worn parts of the knee and replacing the arthritic knee joint with artificial metal (cobalt chrome and titanium) and a plastic (highly cross-linked polyethylene) replacement parts called the 'prostheses'.
The artificial knee joint is made from a surgical-grade metal alloy with a special wear resistant plastic insert.
About Total Knee Replacement Procedure
The procedure is designed to be performed with minimal local trauma
- The knee joint is exposed using a minimally invasive approach
- the damaged portions of the femur and tibia are then cut at the appropriate angles using a high tech intra-operative computerised navigation system
- trial components are then inserted to check the accuracy of these cuts and determine the thickness of plastic required to place in between these two components.
- The patella (kneecap) will need to be resurfaced in most cases. 80% of the natural kneecap is retained
- The real components are then inserted with or without cement and the knee is again checked for implant fit, alignment and stability
- The knee is then carefully closed with dissolving sutures and skin glue. Sterile waterproof dressings and a compression bandage are applied.
Wound Care
Leave any waterproof dressings on your knee until your post-op review.
- You can put all your weight on your leg.
- Put ice on the knee for 20 minutes at a time, as frequently as possible.
Post-op review
The first review will usually be after 10-14 days.
Physiotherapy
You will be seen by a Physiotherapist who will teach you to use crutches and show you some simple exercises to do at home.
Exercise and therapy can begin after a few days or can be arranged at your first post-op visit.
Complications
If you have any redness around the wound or increasing pain in the knee or you have a temperature or feel unwell, you should contact our office or your GP as soon as possible.
Why is Rehabilitation for TKR Essential?
Physiotherapy is an integral part of the treatment and is recommended to start as early as possible. Pre-operative physiotherapy is helpful to better prepare the knee for surgery. The early aim is to regain range of motion, reduce swelling and achieve full weight-bearing.
Sometimes, in-patient rehabilitation is required to regain mobility and independence.
Total Knee Reconstruction - Rehabilitation Program
Treatment Process
After Your Replacement Surgery
After your operation, you will have a drip in your arm for pain medication and antibiotics. You may need between 3-5 nights in the hospital, followed by a stay in a rehabilitation facility. Crutches are required for 1 – 2 weeks following the replacement.
Going Home After Replacement Surgery
Remember to arrange for someone to take you home, as driving is not recommended for several weeks following knee replacement.
Return to Work
You may return to light work duties after 3-4 weeks. You will not be fit to perform work duties that involve:
- prolonged standing,
- heavy lifting,