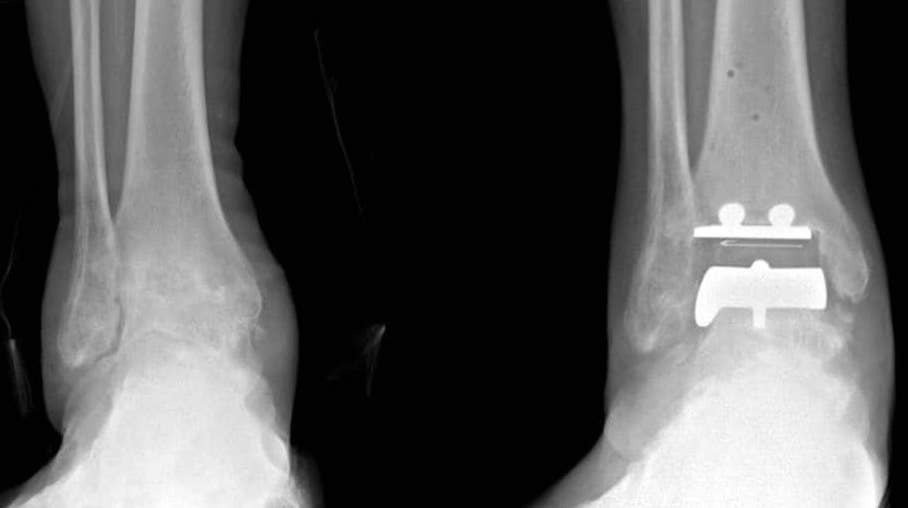
Ankle Joint Replacement
What is Ankle Joint Replacement
Ankle joint replacement, also known as Total Ankle Arthroplasty, is commonly a surgical procedure performed to relieve pain and immobility due to ankle arthritis.
Ankle joint replacement ensures the minimal destruction of the bones and preservation of the other joints of the foot from arthritis, and is advised in low-demand patients.
It also facilitates improved joint motion. However, wear-and-tear of the prosthesis is a major concern with joint replacement, especially in younger patients.
Why Consider Ankle Joint Replacement
Ankle arthritis can be treated with ankle joint replacement surgery, where the diseased joint ends are replaced with metal and plastic prostheses. The causes of ankle arthritis can include:
- Infection,
- Bone fracture,
- Connective tissue disorder,
- Excessive stress, and
- Disease conditions such as rheumatoid arthritis and osteoarthritis.
Indications for Ankle Joint Replacement
Ankle joint replacement is indicated with the following:
- When conservative treatments fail to reduce the pain and joint function
- Recommended for elderly patients with a severe fracture from osteoporosis
- Rheumatoid arthritis
However, the procedure is contraindicated in patients with
- Dead bone in the talus (ankle bone) and significant deformity
- Infections of the ankle (previous or current)
- Significant lower extremity neuropathy
- Inadequate function or loss of leg muscle function
- Poor blood supply to the leg
- Inadequate presence of soft tissues
How Risks Are Minimised
Get Moving Quickly
Early mobilisation is a major preventive measure. We strongly encourage you to get moving and out of bed as soon as possible after the operation to restore normal blood flow in the legs.
You should aim to do at least ten short walks (of between 2 and 5 minutes) each day in the first two weeks after surgery.
How Can I Minimise Post Operative Complications
Blood clots (DVT or PE)
All patients receive a number of treatment measures to reduce the risk of blood clots. These include
- Injections of heparin during and after surgery,
- Sequential calf compression device (SCD) whilst on the operating table, and
- Special leg stockings (TEDS)
As a result of these measures, we have never had a patient develop a deep venous thrombosis. Any patient who is at high risk of a blood clot (such as a history of blood clots or clotting disorders) may be asked to continue heparin (Clexane) injections for 10 days after the surgery in addition to the other measures. This can be done at home, and we will show you how.
What Are the Consequences of Surgery?
Sometimes the potential risks and consequences of your surgical procedure need to be weighed against the benefits of a successful surgical outcome.
Like most surgery these benefits can include:
- Freedom from pain
- Increase movement
- Greater Flexibility,
- Maintained Independence
- Improved outlook, and
- Longer more enjoyable life
Although the recurrence of the presenting problem is not very common, after surgery, you would need to follow preventive measures.
It is important to avoid high impact activities during the early phase of recovery to minimise the risk of further injury. If there are any postoperative concerns or pain, please do not hesitate in contacting our rooms.